Ference及同事开展一系列孟德尔随机化研究,涉及与低密度脂蛋白胆固醇(LDL-C)血清水平相关的6个不同基因的9种多态性。对每种多态性,确定等位基因对LDL-C和冠心病(CHD)风险的影响。
Ference及同事开展一系列孟德尔随机化研究,涉及与低密度脂蛋白胆固醇(LDL-C)血清水平相关的6个不同基因的9种多态性。对每种多态性,确定等位基因对LDL-C和冠心病(CHD)风险的影响。对LDL-C每降低1单位的CHD风险降低,每种等位基因暴露的效应高度一致,无效应异质性的证据。一项包含312 321例参与者数据的荟萃分析发现,长期暴露于较低LDL-C水平时,LDL-C每降低38.7 mg/dl(1 mmol/L),CHD风险降低55%。与生命后期开始他汀治疗所观察到的获益相比,LDL-C每降低1单位的CHD风险多降低三倍。这些结果证实终身低水平LDL-C的益处。
J Am Coll Cardiol.2012;60(25):2631-2639.
点评
降低胆固醇以预防冠心病,越早也好
Lowering cholesterol to prevent coronary heart disease cannot start early enough
Patrick Diemert,MD 德国汉堡大学心脏中心
Jeanette Erdmann,PhD 德国Lubeck大学整合和实验遗传学研究所
The distribution of common genetic polymorphisms during meiosis can roughly be compared to a randomized trial, designed by nature, in which genetic polymorphisms that lower cholesterol will be randomly allocated to individuals at conception. Several previous studies have shown that the association of these polymorphisms with lower cholesterol can already be detected in childhood. As a result, carriers of such cholesterol-lowering alleles will experience genetically determined lowering of cholesterol that will last life-long.
This has led to the concept of Mendelian randomization (MR). A Mendelian randomization has three prerequisites: (A) a genetic polymorphism is associated with a quantitative trait such as LDL-cholesterol levels; (B) the quantitative association between the risk factor and disease risk is known; and (C) a genetic polymorphism is associated with disease risk such as risk of CHD. These three prerequisites can be compared to three sides of a triangle (Figure 8). If A is known and B is known from genetic studies, it is possible to predict disease risk in C. If the observed disease risk in C is equal to the risk predicted by A and B, we can assume that the genetic risk factor is causal for the disease.
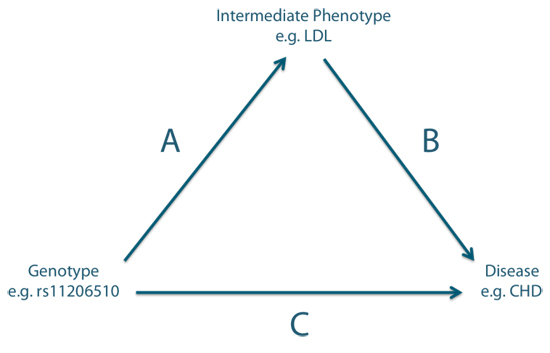
图8 基因型、中间表型和疾病之间的关系
Mendelian randomization experiments have been performed for a number of genetic variants that lower LDL-cholesterol and have consistently implied a causal relationship between genetically lowered LDL-cholesterol and CHD risk. Importantly, such MR experiments have also been carried out for other CHD risk factors such as HDL-cholesterol and C-reactive protein but in these latter cases, no causal association was implied because predicted and observed risk were not equal.
The results of MR studies for various CHD risk factors can be interpreted as follows: While genetic lowering of LDL-cholesterol is causally linked to lower CHD risk, other CHD risk factors such as HDL-cholesterol or C-reactive protein are not causally linked but are secondary to the disease or epi-phenomena not causally related.
The importance of the study by Ference et al. is that a large number of MR studies for LDL have been combined in a single meta-analysis that demonstrated the strong consistency between the previous studies. This meta-analysis also allows the comparison with large-scale clinical trials of LDL-C lowering using statins.
The article by Ference et al has two strong clinical messages:
1.)It nicely demonstrates that the risk reduction with LDL-C lowering achieved if statin therapy is started in adult life is clearly inferior to the risk reduction achieved with life-long LDL-C lowering through genetic polymorphisms. Since, in the clinical trials, the average age for the start of LDL-C lowering was 63 years, this might be much too late. LDL-lowering started at a much younger age should therefore result in a better benefit of therapy.
2.) The study strongly supports that LDL-cholesterol is a causal risk factor for CHD.
In many Western countries, LDL-C lowering using statins is still a matter of controversy, with some members of the medical community even questioning the value of LDL-lowering. Mendelian randomization studies of LDL-lowering send a clear message that there is an unequivocal causal relationship between LDL-levels and coronary heart disease risk and that LDL-lowering that is started early can indeed save lives.
减数分类时常见基因多态性的分布可大致比拟为大自然设计的随机试验,其中降低胆固醇的基因多态性在受孕时被随机分配至个体。既往研究显示,儿童时期即可检测出这些多态性与低胆固醇水平的关联。携带这些降胆固醇等位基因的个体将终生处于遗传学决定的低胆固醇状态。
这种现象引出孟德尔随机化(MR)的概念。MR必须满足三项前提条件:①基因多态性与数量性状例如低密度脂蛋白胆固醇(LDL-C)相关;②已知危险因素和疾病风险的定量联系;③基因多态性与疾病风险例如冠心病风险相关。这三项前提条件类似三角形的三条边(图8)。图中,A表示基因变异与数量性状(如LDL-C)的关联;B表示危险因素与疾病风险的已知关联;C表示遗传变异与疾病风险(如冠心病)的关联。如果从遗传学研究中已知A和B,那么就可能预测C。如果观察到的C疾病风险与从A和B预测的风险相等,我们可假定遗传学风险因素可导致该疾病。
MR试验已就多种降低LDL-C的遗传变异展开研究,一致提示遗传的低LDL-C水平与冠心病风险具因果关系。MR试验也针对其他冠心病危险因素如高密度脂蛋白胆固醇(HDL-C)和C反应蛋白(CRP),但这些研究未提示因果关系,因为预测和观察到的风险不相等。
关于冠心病危险因素的MR研究结果可理解为:遗传学降低LDL-C与低冠心病风险有因果关系;其他危险因素如HDL-C或CRP与冠心病无因果联系,仅为一种没有因果关系的副现象。
Ference和同事的这项研究的重要性在于,该项纳入大量MR研究的荟萃分析证实既往研究的高度一致性。这项荟萃分析还对比MR试验与他汀降LDL-C的大型临床试验。Ference文章的临床意义有两点:①证实生命晚期起始他汀治疗降低LDL-C获得的风险降低,劣于基因多态性所致终生低LDL-C的获益。临床试验中,开始降LDL-C治疗的平均年龄为63岁,可能太晚。更早开始降LDL-C治疗,理应获得更多益处。②强有力支持LDL-C与冠心病有因果关系。
在很多西方国家,使用他汀降低LDL-C仍存争议,一些医学界人士甚至怀疑降LDL-C的意义。降低LDL-C的MR研究明确显示LDL-C水平与冠心病风险之间的因果关系;尽早开始降LDL-C确能挽救生命。



 京公网安备 11010502033353号
京公网安备 11010502033353号